Pancreatic Cancer Treatment (PDQ®): Treatment - Patient Information [NCI]
This information is produced and provided by the National Cancer Institute (NCI). The information in this topic may have changed since it was written. For the most current information, contact the National Cancer Institute via the Internet web site at http://cancer.gov or call 1-800-4-CANCER.
General Information About Pancreatic Cancer
Pancreatic cancer is a type of cancer that forms in the tissues of the pancreas.
The pancreas is a gland about 6 inches long that is shaped like a thin pear lying on its side. The wider end of the pancreas is called the head, the middle section is called the body, and the narrow end is called the tail. The pancreas lies between the stomach and the spine.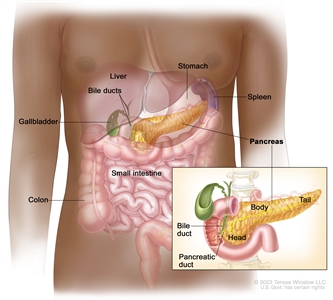
Anatomy of the pancreas. The pancreas has three areas: the head, body, and tail. It is found in the abdomen near the stomach, intestines, and other organs.
The pancreas has two main jobs in the body:
- to make juices that help break down food into substances the body can use
- to make hormones, such as insulin and glucagon, that help control blood sugar levels and help the body use and store the energy it gets from food
Pancreatic cancer can occur in exocrine pancreas cells, which produce digestive juices, or the endocrine pancreas cells, which produce hormones. About 95% of pancreatic cancers begin in exocrine cells.
This summary is about exocrine pancreatic cancer. For information about endocrine pancreatic cancer, see Pancreatic Neuroendocrine Tumors (Islet Cell Tumors) Treatment.
Smoking and health history can affect the risk of pancreatic cancer.
Pancreatic cancer is caused by certain changes to the way pancreatic cells function, especially how they grow and divide into new cells. A risk factor is anything that increases the chance of getting a disease. Some risk factors for pancreatic cancer, like smoking, can be changed. However, risk factors also include things people cannot change, like their genetics and their family history. Learning about risk factors for pancreatic cancer can help you make changes that might lower your risk of getting it.
There are many risk factors for pancreatic cancer, but many do not directly cause cancer. Instead, they increase the chance of DNA damage in cells that may lead to pancreatic cancer. To learn more about how cancer develops, see What Is Cancer?
Having one or more of these risk factors does not mean that you will get pancreatic cancer. Many people with risk factors never develop pancreatic cancer, while others with no known risk factors do.
Risk factors for pancreatic cancer include:
- smoking
- having excess body weight
- having a personal history of diabetes or chronic pancreatitis
- having a family history of pancreatic cancer or pancreatitis
- having certain hereditary conditions, such as:
- multiple endocrine neoplasia type 1 (MEN1) syndrome
- hereditary nonpolyposis colon cancer (HNPCC; Lynch syndrome)
- von Hippel-Lindau syndrome
- Peutz-Jeghers syndrome
- hereditary breast and ovarian cancer syndrome
- familial atypical multiple mole melanoma (FAMMM) syndrome
- ataxia-telangiectasia
Talk with your doctor if you think you might be at risk.
Signs and symptoms of pancreatic cancer include jaundice, pain, and weight loss.
Early on, pancreatic cancer may not cause any signs or symptoms, making it hard to detect. As the cancer grows, symptoms may include:
- jaundice (yellowing of the skin and whites of the eyes)
- light-colored stools
- dark urine
- pain in the upper or middle abdomen and back
- weight loss for no known reason
- loss of appetite
- fatigue
These symptoms may be caused by many conditions other than pancreatic cancer. It's important to check with your doctor if you have any of these symptoms to find out the cause and begin treatment, if needed.
Pancreatic cancer is difficult to diagnose early.
Pancreatic cancer is difficult to detect and diagnose for the following reasons:
- There aren't any noticeable signs or symptoms in the early stages of pancreatic cancer.
- The signs and symptoms of pancreatic cancer, when present, are like the signs and symptoms of many other illnesses.
- The pancreas is hidden behind other organs such as the stomach, small intestine, liver, gallbladder, spleen, and bile ducts.
Tests that examine the pancreas are used to diagnose and stage pancreatic cancer.
Pancreatic cancer is usually diagnosed with tests and procedures that make pictures of the pancreas and the area around it. The process used to find out if cancer cells have spread within and around the pancreas is called staging. Tests and procedures to detect, diagnose, and stage pancreatic cancer are usually done at the same time. To plan treatment, it is important to know the stage of the disease and whether the pancreatic cancer can be removed by surgery.
In addition to asking about your personal and family health history and doing a physical exam, your doctor may perform the following tests and procedures:
- Blood chemistry study is a laboratory test in which a blood sample is checked to measure the amounts of certain substances, such as bilirubin, released into the blood by organs and tissues in the body. An unusual (higher or lower than normal) amount of a substance can be a sign of disease.
- Tumor marker test checks a sample of blood, urine, or tissue to measure the amounts of certain substances, such as CA 19-9 and carcinoembryonic antigen (CEA), made by organs, tissues, or tumor cells in the body. Certain substances are linked to specific types of cancer when found in increased levels in the body. These are called tumor markers.
- MRI (magnetic resonance imaging) uses a magnet, radio waves, and a computer to make a series of detailed pictures of areas inside the body. This procedure is also called nuclear magnetic resonance imaging (NMRI).
- CT scan (CAT scan) uses a computer linked to an x-ray machine to make a series of detailed pictures of areas inside the body. The pictures are taken from different angles and are used to create 3-D views of tissues and organs. A dye may be injected into a vein or swallowed to help the organs or tissues show up more clearly. This procedure is also called computed tomography, computerized tomography, or computerized axial tomography. A spiral or helical CT scan makes a series of very detailed pictures of areas inside the body using an x-ray machine that scans the body in a spiral path.
- PET scan (positron emission tomography scan) uses a small amount of radioactive sugar (also called glucose) that is injected into a vein. Then a scanner rotates around the body to make detailed, computerized pictures of areas inside the body where the glucose is taken up. Because cancer cells often take up more glucose than normal cells, the pictures can be used to find cancer cells in the body. A PET scan and CT scan may be done at the same time. This is called a PET-CT.
- Abdominal ultrasound makes pictures of the inside of the abdomen. The ultrasound transducer is pressed against the skin of the abdomen and directs high-energy sound waves (ultrasound) into the abdomen. The sound waves bounce off the internal tissues and organs and make echoes. The transducer receives the echoes and sends them to a computer, which uses the echoes to make pictures called sonograms.
- Endoscopic ultrasound (EUS) is a procedure that uses an endoscope inserted into the body, usually through the mouth or rectum. An endoscope is a thin, tube-like instrument with a light and a lens for viewing. A probe at the end of the endoscope is used to bounce high-energy sound waves (ultrasound) off internal tissues or organs and make echoes. The echoes form a picture of body tissues called a sonogram. This procedure is also called endosonography.
- Endoscopic retrograde cholangiopancreatography (ERCP) is a procedure to x-ray the ducts (tubes) that carry bile from the liver to the gallbladder and from the gallbladder to the small intestine. Sometimes pancreatic cancer causes these ducts to narrow and block or slow the flow of bile, causing jaundice. An endoscope (a thin, lighted tube) is passed through the mouth, esophagus, and stomach into the first part of the small intestine. A catheter (a smaller tube) is then inserted through the endoscope into the pancreatic ducts. A dye is injected through the catheter into the ducts and an x-ray is taken. If the ducts are blocked by a tumor, a fine tube may be inserted into the duct to unblock it. This tube (or stent) may be left in place to keep the duct open. Tissue samples may also be taken.
- Percutaneous transhepatic cholangiography (PTC) is a procedure to x-ray the liver and bile ducts. A thin needle is inserted through the skin below the ribs and into the liver. Dye is injected into the liver or bile ducts and an x-ray is taken. If a blockage is found, a thin, flexible tube called a stent is sometimes left in the liver to drain bile into the small intestine or a collection bag outside the body. This test is done only if ERCP cannot be done.
- Laparoscopy is a surgical procedure to look at the organs inside the abdomen to check for signs of disease. Small incisions (cuts) are made in the wall of the abdomen and a laparoscope (a thin, lighted tube) is inserted into one of the incisions. The laparoscope may have an ultrasound probe at the end in order to bounce high-energy sound waves off internal organs, such as the pancreas. This is called laparoscopic ultrasound. Other instruments may be inserted through the same or other incisions to perform procedures such as taking tissue samples from the pancreas or a sample of fluid from the abdomen to check for cancer.
- Biopsy is the removal of cells or tissues so they can be viewed under a microscope by a pathologist to check for signs of cancer. There are several ways to do a biopsy for pancreatic cancer. A fine needle or a core needle may be inserted into the pancreas during an x-ray or ultrasound to remove cells. Tissue may also be removed during a laparoscopy or surgery to remove the tumor.
Some people decide to get a second opinion.
You may want to get a second opinion to confirm your pancreatic cancer diagnosis and treatment plan. If you seek a second opinion, you will need to get medical test results and reports from the first doctor to share with the second doctor. The second doctor will review the pathology report, slides, and scans. They may agree with the first doctor, suggest changes or another treatment approach, or provide more information about your cancer.
To learn more about choosing a doctor and getting a second opinion, see Finding Cancer Care. You can contact NCI's Cancer Information Service via chat, email, or phone (both in English and Spanish) for help finding a doctor, hospital, or getting a second opinion. For questions you might want to ask at your appointments, see Questions to Ask Your Doctor about Cancer.
Certain factors affect prognosis (chance of recovery) and treatment options.
The prognosis and treatment options depend on:
- whether the tumor can be removed by surgery
- the stage of the cancer (the size of the tumor and whether the cancer has spread outside the pancreas to nearby tissues or lymph nodes or to other places in the body)
- the patient's general health
- whether the cancer has just been diagnosed or has recurred (come back)
Pancreatic cancer can be controlled only if it is found before it has spread, when it can be completely removed by surgery. If the cancer has spread, palliative treatment can improve the patient's quality of life by controlling the symptoms and complications of this disease.
Stages of Pancreatic Cancer
Cancer stage describes the extent of cancer in the body.
Cancer stage describes the extent of cancer in the body, such as the size of the tumor, whether it has spread, and how far it has spread from where it first formed. It is important to know the stage of the pancreatic cancer to plan the best treatment.
There are several staging systems for cancer that describe the extent of the cancer. Pancreatic cancer staging usually uses the TNM staging system. You may see your cancer described by this staging system in your pathology report. Based on the TNM results, a stage (I, II, III, or IV, also written as 1, 2, 3, or 4) is assigned to your cancer. When talking to you about your cancer, your doctor may describe it as one of these stages.
To learn how doctors stage pancreatic cancer, see tests to diagnose and stage pancreatic cancer. Learn more about Cancer Staging.
The information in this section is about staging for exocrine pancreatic cancer, the most common type of pancreatic cancer.
The following stages are used for pancreatic cancer:
Stage 0 (carcinoma in situ)
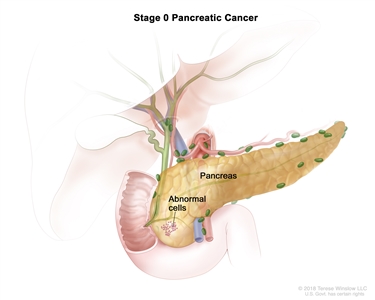
Stage 0 pancreatic cancer. Abnormal cells are found in the lining of the pancreas. These abnormal cells may become cancer and spread into nearby normal tissue.
In stage 0, abnormal cells are found in the lining of the pancreas. These abnormal cells may become cancer and spread into nearby normal tissue. Stage 0 is also called carcinoma in situ.
Stage I (also called stage 1) pancreatic cancer
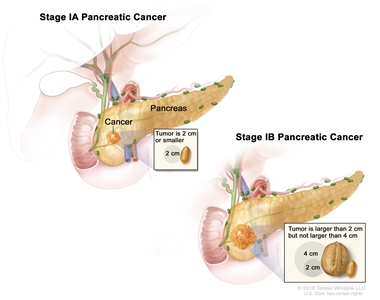
Stage I pancreatic cancer. Cancer is found in the pancreas only. In stage IA, the tumor is 2 centimeters or smaller. In stage IB, the tumor is larger than 2 centimeters but not larger than 4 centimeters.
In stage I, cancer has formed and is found in the pancreas only. Stage I is divided into stages IA and IB, depending on the size of the tumor.
- Stage IA: The tumor is 2 centimeters or smaller.
- Stage IB: The tumor is larger than 2 centimeters but not larger than 4 centimeters.
Stage II (also called stage 2) pancreatic cancer
Stage II is divided into stages IIA and IIB, depending on the size of the tumor and where the cancer has spread.
- Stage IIA: The tumor is larger than 4 centimeters.
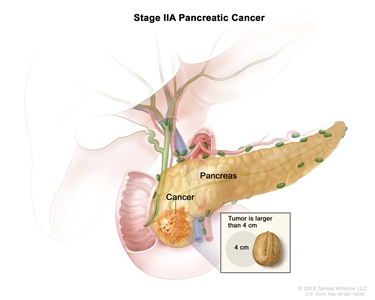
Stage IIA pancreatic cancer. The tumor is larger than 4 centimeters. - Stage IIB: The tumor is any size, and cancer has spread to 1 to 3 nearby lymph nodes.
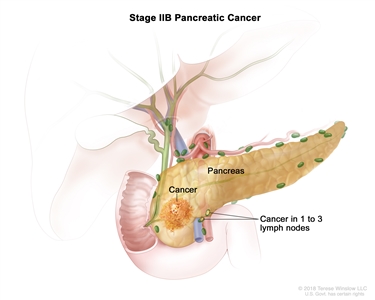
Stage IIB pancreatic cancer. The tumor is any size and cancer has spread to 1 to 3 nearby lymph nodes.
Stage III (also called stage 3) pancreatic cancer
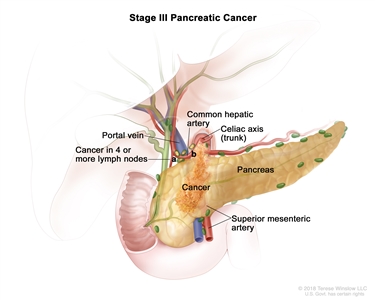
Stage III pancreatic cancer. The tumor is any size and cancer has spread to (a) 4 or more nearby lymph nodes; or (b) the major blood vessels near the pancreas. These include the portal vein, common hepatic artery, celiac axis (trunk), and superior mesenteric artery.
In stage III, the tumor is any size, and cancer has spread to:
- four or more nearby lymph nodes; or
- the major blood vessels near the pancreas.
Stage IV (also called stage 4) pancreatic cancer
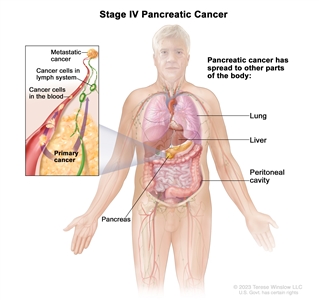
Stage IV pancreatic cancer. The tumor is any size and cancer has spread to other parts of the body, such as the lung, liver, or peritoneal cavity (the body cavity that contains most of the organs in the abdomen).
In stage IV, the tumor is any size, and cancer has spread to other parts of the body, such as the liver, lung, or peritoneal cavity (the body cavity that contains most of the organs in the abdomen).
Stage IV pancreatic cancer is also called metastatic pancreatic cancer. Metastatic cancer happens when cancer cells travel through the lymphatic system or blood and form tumors in other parts of the body. The metastatic tumor is the same type of cancer as the primary tumor. For example, if pancreatic cancer spreads to the liver, the cancer cells in the liver are actually pancreatic cancer cells. The disease is called metastatic pancreatic cancer, not liver cancer. Learn more in Metastatic Cancer: When Cancer Spreads.
The following groups are used to plan treatment:
Resectable pancreatic cancer
Resectable pancreatic cancer can be removed by surgery because it has not grown into major blood vessels near the tumor.
Borderline resectable pancreatic cancer
Borderline resectable pancreatic cancer has grown into a major blood vessel or nearby tissue or organs. It may be possible to remove the tumor, but there is a high risk that all of the cancer cells will not be removed with surgery.
Locally advanced pancreatic cancer
Locally advanced pancreatic cancer has grown into or close to nearby lymph nodes or blood vessels, so surgery cannot completely remove the cancer.
Metastatic pancreatic cancer
Metastatic pancreatic cancer has spread to other organs, so surgery cannot completely remove the cancer.
Recurrent pancreatic cancer
Recurrent pancreatic cancer is cancer that has recurred (come back) after it has been treated. The cancer may come back in the pancreas or in other parts of the body. Tests will be done to help determine where the cancer has returned in your body. The type of treatment for recurrent pancreatic cancer will depend on where it has come back.
Learn more in Recurrent Cancer: When Cancer Comes Back. Information to help you cope and talk with your health care team can be found in the booklet When Cancer Returns.
Treatment Option Overview
There are different types of treatment for patients with pancreatic cancer.
Different types of treatments are available for people with pancreatic cancer. You and your cancer care team will work together to decide your treatment plan, which may include more than one type of treatment. Many factors will be considered, such as the stage of the cancer, your overall health, and your preferences. Your plan will include information about your cancer, the goals of treatment, your treatment options and the possible side effects, and the expected length of treatment.
Talking with your cancer care team before treatment begins about what to expect will be helpful. You'll want to learn what you need to do before treatment begins, how you'll feel while going through it, and what kind of help you will need. To learn more, see Questions to Ask Your Doctor about Treatment.
The following types of treatment are used:
Surgery
One of the following types of surgery may be used to take out the tumor:
- Whipple procedure is surgery to remove the head of the pancreas, the gallbladder, part of the stomach, part of the small intestine, and the bile duct. Enough of the pancreas is left to produce digestive juices and insulin.
- Total pancreatectomy is surgery to remove the whole pancreas, part of the stomach, part of the small intestine, the common bile duct, the gallbladder, the spleen, and nearby lymph nodes.
- Distal pancreatectomy is surgery to remove the body and the tail of the pancreas. The spleen may also be removed if cancer has spread to the spleen.
If the cancer has spread and cannot be removed, the following types of palliative surgery may be done to relieve symptoms and improve quality of life:
- Biliary bypass: If cancer is blocking the bile duct and bile is building up in the gallbladder, a biliary bypass may be done. During this operation, the doctor will cut the gallbladder or bile duct in the area before the blockage and sew it to the small intestine to create a new pathway around the blocked area.
- Endoscopic stent placement: If the tumor is blocking the bile duct, surgery may be done to put in a stent (a thin tube) to drain bile that has built up in the area. The doctor may place the stent through a catheter that drains the bile into a bag on the outside of the body, or the stent may go around the blocked area and drain the bile into the small intestine.
- Gastric bypass: If the tumor is blocking the flow of food from the stomach, the stomach may be sewn directly to the small intestine so the patient can continue to eat normally.
Radiation therapy
Radiation therapy uses high-energy x-rays or other types of radiation to kill cancer cells or keep them from growing. Pancreatic cancer is sometimes treated with external beam radiation therapy. This type of radiation therapy uses a machine outside the body to send radiation toward the area of the body with cancer.
Learn more about External Beam Radiation Therapy for Cancer and Radiation Therapy Side Effects.
Chemotherapy
Chemotherapy (also called chemo) uses drugs to stop the growth of cancer cells, either by killing the cells or by stopping them from dividing.
Chemotherapy for pancreatic cancer is usually systemic, meaning it is injected into a vein or given by mouth. When given this way, the drugs enter the bloodstream to reach cancer cells throughout the body.
Chemotherapy drugs used to treat pancreatic cancer may include:
- capecitabine
- fluorouracil (5-FU)
- gemcitabine
- irinotecan
- irinotecan sucrosofate (also called nanoliposomal irinotecan)
- leucovorin (a vitamin that improves the effectiveness of 5-FU)
- oxaliplatin
Combinations of these drugs may be used. Other chemotherapy drugs not listed here may also be used.
Chemotherapy may also be combined with other kinds of treatment. For example, it may be combined with radiation therapy or targeted therapy.
Learn more about how chemotherapy works, how it is given, common side effects, and more at Chemotherapy to Treat Cancer and Chemotherapy and You: Support for People With Cancer.
Chemoradiation therapy
Chemoradiation therapy combines chemotherapy and radiation therapy to increase the effects of both.
Targeted therapy
Targeted therapy uses drugs or other substances to identify and attack specific cancer cells. Erlotinib is a targeted therapy drug used to treat pancreatic cancer.
Learn more about Targeted Therapy to Treat Cancer.
There are treatments for pain caused by pancreatic cancer.
Pain can occur when the tumor presses on nerves or other organs near the pancreas. When pain medicine is not enough, there are treatments that act on nerves in the abdomen to relieve the pain. The doctor may inject medicine into the area around affected nerves or may cut the nerves to block the feeling of pain. Radiation therapy with or without chemotherapy can also help relieve pain by shrinking the tumor. Learn more about Cancer Pain.
Patients with pancreatic cancer have special nutritional needs.
Surgery to remove the pancreas may affect its ability to make pancreatic enzymes that help to digest food. As a result, patients may have problems digesting food and absorbing nutrients into the body. To prevent malnutrition, the doctor may prescribe medicines that replace these enzymes.
New types of treatment are being tested in clinical trials.
For some people, joining a clinical trial may be an option. There are different types of clinical trials for people with cancer. For example, a treatment trial tests new treatments or new ways of using current treatments. Supportive care and palliative care trials look at ways to improve quality of life, especially for those who have side effects from cancer and its treatment.
You can use the clinical trial search to find NCI-supported cancer clinical trials accepting participants. The search allows you to filter trials based on the type of cancer, your age, and where the trials are being done. Clinical trials supported by other organizations can be found on the ClinicalTrials.gov website.
Learn more about clinical trials, including how to find and join one, at Clinical Trials Information for Patients and Caregivers.
Treatment for pancreatic cancer may cause side effects.
For information about side effects caused by treatment for cancer, visit our Side Effects page.
Follow-up care may be needed.
As you go through treatment, you will have follow-up tests or check-ups. Some tests that were done to diagnose or stage the cancer may be repeated to see how well the treatment is working. Decisions about whether to continue, change, or stop treatment may be based on the results of these tests.
Some of the tests will continue to be done from time to time after treatment has ended. The results of these tests can show if your condition has changed or if the cancer has recurred (come back).
Treatment of Resectable or Borderline Resectable Pancreatic Cancer
Treatment of resectable or borderline resectable pancreatic cancer may include:
- chemotherapy with or without radiation therapy, followed by surgery
- surgery
- surgery, followed by chemotherapy
- surgery, followed by chemoradiation
- a clinical trial of chemotherapy and/or radiation therapy before surgery
- a clinical trial of chemoradiation, followed by surgery and then chemotherapy
- a clinical trial of different ways of giving radiation therapy
Surgery to remove the tumor may include Whipple procedure, total pancreatectomy, or distal pancreatectomy.
Palliative therapy can be started at any stage of disease. See the Palliative Therapy section for information about treatments that may improve quality of life or relieve symptoms in people with pancreatic cancer.
Learn more about these treatments in the Treatment Option Overview.
Use our clinical trial search to find NCI-supported cancer clinical trials that are accepting patients. You can search for trials based on the type of cancer, the age of the patient, and where the trials are being done. General information about clinical trials is also available.
Treatment of Locally Advanced Pancreatic Cancer
Treatment of pancreatic cancer that is locally advanced may include:
- chemotherapy with or without targeted therapy
- chemotherapy and chemoradiation
- surgery (Whipple procedure, total pancreatectomy, or distal pancreatectomy)
- palliative surgery or stent placement to bypass blocked areas in ducts or the small intestine, and possibly chemotherapy and chemoradiation to shrink the tumor to allow for surgery
- a clinical trial of new anticancer therapies together with chemotherapy or chemoradiation
- a clinical trial of radiation therapy given during surgery or internal radiation therapy
Palliative therapy can be started at any stage of disease. See the Palliative Therapy section for information about treatments that may improve quality of life or relieve symptoms in patients with pancreatic cancer.
Learn more about these treatments in the Treatment Option Overview.
Use our clinical trial search to find NCI-supported cancer clinical trials that are accepting patients. You can search for trials based on the type of cancer, the age of the patient, and where the trials are being done. General information about clinical trials is also available.
Treatment of Metastatic or Recurrent Pancreatic Cancer
Treatment of pancreatic cancer that has metastasized or recurred may include:
- chemotherapy with or without targeted therapy
- clinical trials of new anticancer agents with or without chemotherapy
Palliative therapy can be started at any stage of disease. See the Palliative Therapy section for information about treatments that may improve quality of life or relieve symptoms in patients with pancreatic cancer.
Learn more about these treatments in the Treatment Option Overview.
Use our clinical trial search to find NCI-supported cancer clinical trials that are accepting patients. You can search for trials based on the type of cancer, the age of the patient, and where the trials are being done. General information about clinical trials is also available.
Palliative Therapy
Palliative therapy can improve the patient's quality of life by controlling the symptoms and complications of pancreatic cancer.
Palliative therapy for pancreatic cancer may include:
- palliative surgery or stent placement to bypass blocked areas in ducts or the small intestine
- palliative radiation therapy to help relieve pain by shrinking the tumor
- an injection of medicine to help relieve pain by blocking nerves in the abdomen
- other palliative medical care alone
Learn more about these treatments in the Treatment Option Overview.
Use our clinical trial search to find NCI-supported cancer clinical trials that are accepting patients. You can search for trials based on the type of cancer, the age of the patient, and where the trials are being done. General information about clinical trials is also available.
To Learn More About Pancreatic Cancer
For more information from the National Cancer Institute about pancreatic cancer, see:
- Pancreatic Cancer Home Page
- Childhood Pancreatic Cancer Treatment
- Drugs Approved for Pancreatic Cancer
For general cancer information and other resources from the National Cancer Institute, visit:
About This PDQ Summary
About PDQ
Physician Data Query (PDQ) is the National Cancer Institute's (NCI's) comprehensive cancer information database. The PDQ database contains summaries of the latest published information on cancer prevention, detection, genetics, treatment, supportive care, and complementary and alternative medicine. Most summaries come in two versions. The health professional versions have detailed information written in technical language. The patient versions are written in easy-to-understand, nontechnical language. Both versions have cancer information that is accurate and up to date and most versions are also available in Spanish.
PDQ is a service of the NCI. The NCI is part of the National Institutes of Health (NIH). NIH is the federal government's center of biomedical research. The PDQ summaries are based on an independent review of the medical literature. They are not policy statements of the NCI or the NIH.
Purpose of This Summary
This PDQ cancer information summary has current information about the treatment of adult pancreatic cancer. It is meant to inform and help patients, families, and caregivers. It does not give formal guidelines or recommendations for making decisions about health care.
Reviewers and Updates
Editorial Boards write the PDQ cancer information summaries and keep them up to date. These Boards are made up of experts in cancer treatment and other specialties related to cancer. The summaries are reviewed regularly and changes are made when there is new information. The date on each summary ("Updated") is the date of the most recent change.
The information in this patient summary was taken from the health professional version, which is reviewed regularly and updated as needed, by the PDQ Adult Treatment Editorial Board.
Clinical Trial Information
A clinical trial is a study to answer a scientific question, such as whether one treatment is better than another. Trials are based on past studies and what has been learned in the laboratory. Each trial answers certain scientific questions in order to find new and better ways to help cancer patients. During treatment clinical trials, information is collected about the effects of a new treatment and how well it works. If a clinical trial shows that a new treatment is better than one currently being used, the new treatment may become "standard." Patients may want to think about taking part in a clinical trial. Some clinical trials are open only to patients who have not started treatment.
Clinical trials can be found online at NCI's website. For more information, call the Cancer Information Service (CIS), NCI's contact center, at 1-800-4-CANCER (1-800-422-6237).
Permission to Use This Summary
PDQ is a registered trademark. The content of PDQ documents can be used freely as text. It cannot be identified as an NCI PDQ cancer information summary unless the whole summary is shown and it is updated regularly. However, a user would be allowed to write a sentence such as "NCI's PDQ cancer information summary about breast cancer prevention states the risks in the following way: [include excerpt from the summary]."
The best way to cite this PDQ summary is:
PDQ® Adult Treatment Editorial Board. PDQ Pancreatic Cancer Treatment. Bethesda, MD: National Cancer Institute. Updated <MM/DD/YYYY>. Available at: https://www.cancer.gov/types/pancreatic/patient/pancreatic-treatment-pdq. Accessed <MM/DD/YYYY>. [PMID: 26389396]
Images in this summary are used with permission of the author(s), artist, and/or publisher for use in the PDQ summaries only. If you want to use an image from a PDQ summary and you are not using the whole summary, you must get permission from the owner. It cannot be given by the National Cancer Institute. Information about using the images in this summary, along with many other images related to cancer can be found in Visuals Online. Visuals Online is a collection of more than 3,000 scientific images.
Disclaimer
The information in these summaries should not be used to make decisions about insurance reimbursement. More information on insurance coverage is available on Cancer.gov on the Managing Cancer Care page.
Contact Us
More information about contacting us or receiving help with the Cancer.gov website can be found on our Contact Us for Help page. Questions can also be submitted to Cancer.gov through the website's E-mail Us.
Last Revised: 2024-08-28
If you want to know more about cancer and how it is treated, or if you wish to know about clinical trials for your type of cancer, you can call the NCI's Cancer Information Service at 1-800-422-6237, toll free. A trained information specialist can talk with you and answer your questions.


